A Day in the Life of Two Music Therapists
A day in the life of two music therapists
Within Golisano Children’s Hospital’s music therapy program, Rosemary Obi and Elaine Kong use music to help young people get through difficult times

Rosie Obi with a 17-year-old patient
Rosemary “Rosie” Obi, music therapist and internship director for Golisano’s music therapy program, joined the hospital 20 years ago. It was her first job after graduating from the University of Dayton’s music therapy program.
Elaine Kong joined Obi five years ago and focuses on bringing music therapy to the intensive care units for neonatal and pediatric patients, while Obi takes care of patients on the general care units. Together, they provide music therapy for pediatric patients with cancer, blood disorders, heart disease, eating disorders, prematurity, and more.
The program relies and thrives on donor support. Although insurance doesn’t cover the cost of music therapy in the hospital, the Department of Pediatrics is committed to providing it to families at no cost. “Bringing comfort to children and families through song and music-making is vital to the health and well-being of our young patients,” says Obi. “Donor generosity is critical—we are hoping that more people come on board to support it.”
For Obi and Kong, each day is different and includes working with patients, supervising student interns, attending interdisciplinary team rounds, writing notes, and more. Current funding supports a 40-hour week for Obi and a 25-hour week for Kong. Here’s a snapshot of just one of their days.
9:30 a.m.
Obi arrives at her Golisano Children’s Hospital office. She checks in with Kong and the two music therapy interns, then reviews patient charts and sees that, so far, the hospital team—doctors, nurses, and child life specialists–have asked for music therapy services for six new patients in addition to the 50 patients already on their combined caseload.
Obi first sees Sophie*, a 13-year old girl who is finishing up bone cancer treatment–her last chemotherapy session. “When someone reaches a milestone like this, we usually meet them in the hospital lobby where they ring a bell and staff sings them a song about completing treatment,” Obi says. “But, because of COVID-19, we can’t do that.” Instead, Sophie’s care team visits her room before she gets discharged. Obi plays guitar and leads them in song. Sophie beams with happiness and pride—so do her parents.
10:30 a.m.
In the Pediatric Intensive Care Unit, Kong sees Jack*, a three-month-old who suffers from severe bronchopulmonary dysplasia and will enter the foster care system soon. “Jack has to go through some very hard medical procedures—and he has to do it mostly alone,” she says. “I’m lucky that I get to be part of his treatment.”
Because of COVID-19, there are no volunteers and Jack is only seen—and held—by his care team. While the nurses care for Jack, Kong hums, plays the guitar, and sings to him. Although he sleeps through most of this time, his eyes open up here and there and he smiles a few times—a good sign.
11 a.m.
Meanwhile, Obi picks up her guitar and instrument tote, which is full of drums, shakers, tambourines, and more, and is on her way to see Sam*, a three-year-old who’s just been diagnosed with appendicitis. In the elevator, someone asks her if she is about to give a concert.
“Sometimes that happens,” Obi says. “That kind of well-meaning comment actually gives us a chance to clear up a misunderstanding of our role and let people know that we are not entertainers—we are highly trained board-certified music therapists who are part of our patients’ treatment team. We use live music and a variety of techniques to soothe patients, help them develop coping skills, give them a means of expression, and build problem solving skills.” Kong adds that, similar to occupational and physical therapists, music therapists are allied professionals who play a key role within a patient’s care team.
Obi then makes her way to Sam. Wrapped in his mother’s arms, he is very shy and won’t look at Obi. That dynamic soon changes though. After a few minutes of Obi playing some gentle music on her guitar, Sam unfolds from his mother. He sits up, starts talking, smiles, and sings with Obi. By the end of the session, Sam doesn’t want her to leave.
12 p.m.
Obi returns to her office to revisit patient charts, eat lunch, and check the status of the interns. To date, the program has trained 32 practicum students and 37 interns from Nazareth College’s music therapy program, from which Obi received her master’s in creative arts therapy, with a specialization in music therapy, and Kong obtained her bachelor’s in music therapy. She then went on to get her master’s in music therapy from Florida State University before returning to Rochester to work.
1 p.m.
Kong is now in the Neonatal Intensive Care Unit with Derek*, who was born at 27 weeks gestation and is now five weeks old. He started music therapy four weeks ago and is now ready for a new intervention to help him learn how to tolerate different types of stimulation. Kong guides his mother through the intervention and teaches her the technique, which includes humming or singing while massaging and rocking Derek. “He was opening his eyes and smiling throughout the session, while also bonding with his mother,” Kong says. “His mother was happy he received therapy that was so developmentally appropriate for him.”
1:30 p.m.
As part of Golisano’s adolescent medicine team for eating disorders, Obi visits Eliza*, a 16-year-old with anorexia nervosa who was admitted for medical stabilization. Obi tells her about music therapy. To help with Eliza’s anxiety, Obi leads her through an art activity based on music listening. She also guides her through some progressive muscle relaxation and breathing techniques combined with music. Obi often uses mindfulness and music with older youth who are in a lot of mental or emotional pain.
Obi also suggests that Eliza create a soundtrack for her life. She asks Eliza, “if your life were a movie, which songs would you include?” Obi notes that it’s a starting point for them to make a connection and for Eliza to find a new way to express herself and what’s meaningful to her.
2:15 p.m.
Kong is called to be present while one of her patients receives an echocardiogram. The test is almost done, but the toddler starts to panic. Luckily, Kong arrived before the care team was about to medicate her. “I came in and started singing one of her favorite songs,” she says. “It calmed her down and she didn’t need that extra medication after all—a successful musical intervention.” She returns to her office afterward to write chart notes and document each patient’s progress. Kong reflects at the end of the day, “I love my job–I get to do what I love and bring the power of music to very young people who are in very difficult situations.”
3:30 p.m.
Obi sees a medically complex patient, as she, Kong, and the interns often do. These are young people with multiple diagnoses. In this case, Marcos*, an 8-year old child with cerebral palsy and pneumonia, has just been admitted. Obi spends time with him to see how he responds to music. She brings along her guitar and instrument tote to see what he likes. She helps him play the cabasa, a small beaded instrument that provides him some tactile stimulation while she sings familiar and improvised songs. She will continue to work with the child life specialist, along with his occupational and physical therapist, to develop a plan to improve his fine motor skills and meet his developmental needs.
4:45 p.m.
Obi sees her final patient of the day. Maya is a 12-year-old with end stage renal disease who is admitted for a painful urinary tract infection. Obi has known Maya since her first admission for kidney disease 10 years ago. Today, Maya shares her disappointment that she is missing out on a school event. Her parents leave the room and give their daughter some privacy.
Maya then writes a song about how she is feeling. Obi provides suggestions, validates her thoughts and feelings, and helps Maya decide how the song should sound. She also works with her to develop a guitar accompaniment. Maya listens to her finished song with pride and sings along quietly. When her parents return to the room 45 minutes later, Maya shares the recording with them. Within the lyrics, Maya expresses frustration followed by thoughts of hope, strength, and resilience, which her parents recognize and remind her of often. The family has tears in their eyes as they discuss sharing the song for others to hear.
5:30 p.m.
Obi returns to her office to write chart notes and review intern notes. It’s not unusual for her to stay past 6 p.m. to make sure she sees as many patients as possible. “No day is the same,” she says. “It’s always interesting and I am always learning. And, most importantly, it’s such a gift to bring music into our patients’ and their families’ lives and do it in a therapeutic way.”
What is music therapy?
Music therapy uses music to promote healing and enhance quality of life. It complements medical treatments and helps patients cope mentally and physically with their diagnosis. Music therapy may involve listening to music, making music, singing, and discussing music, along with guided imagery with music. It helps ease stress, fear, and anxiety; improves mood; lowers heart rate; alleviates depression; aids with sleep; and provides relaxation. It gives young patients so much of what they need to deal with their circumstances.

Jorie Pucillo with Rosie Obi and a nurse
Thank you, music therapy
Patients and families like the Pucillos are grateful for music therapy. In the spring of 2020, Jorie Pucillo, a three-year-old with Down Syndrome, was diagnosed with leukemia. Unfortunately, Jorie was no stranger to the hospital. When she was six months old, she endured open heart surgery. For her cancer diagnosis, she went through six rounds of chemotherapy and was in the hospital for six months. During each round of chemo, she had music therapy.
“Rosie Obi was awesome—she came in, sang, played guitar, and even showed Jorie how to play the ukulele,” says Jorie’s father, Jerry, a musician who also participated in the music therapy sessions. “Every time Rosie came into the room, Jorie’s mood changed. She was able to play and have a sense of normalcy even when she was in the hospital for so long.”

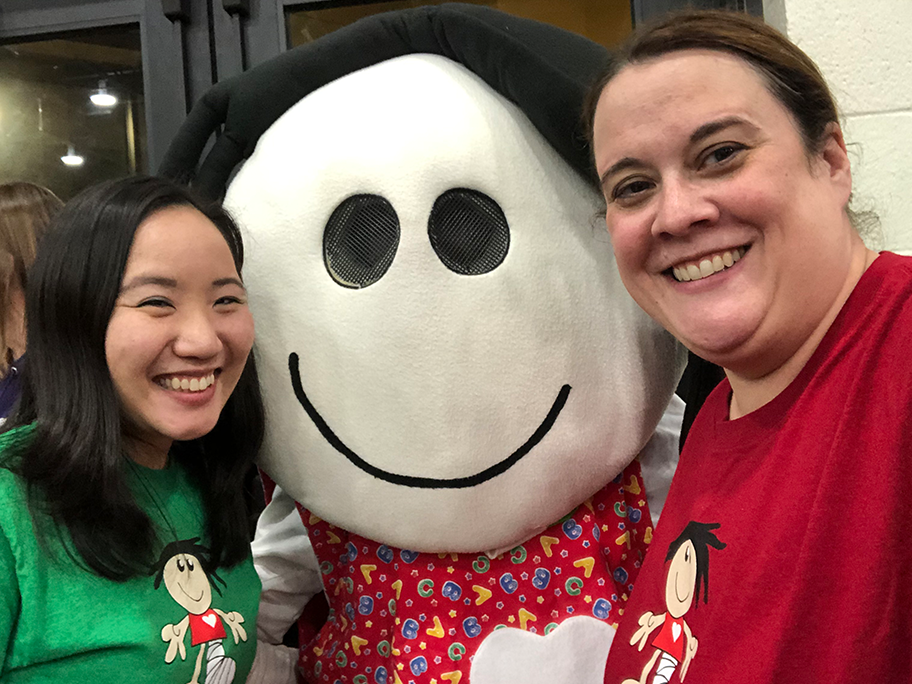
Rachel Wilson (center, holding check), Elaine Kong (in green), Rosie Obi (behind Kong), Morgan Kowalski (in orange), Sandy Strong, and other supporters at the Battle of the Beaks.
Going full circle for music therapy
Rachel Wilson was born with a diaphragmatic hernia, a rare condition that put her the NICU for four months after birth. Today, although she only has 60 percent lung capacity, she is thriving. Wilson just graduated from Nazareth College where she was a nursing student and a lacrosse player. Soon, she will start a nursing job in the NICU at Golisano.
While at Nazareth, Wilson was actively involved in the school’s annual “Battle of the Beaks” fundraiser. Every year (except during the pandemic), when Nazareth’s basketball team plays the St. John Fisher’s Cardinals, ticket sales, concessions, and raffles all benefit Golisano’s music therapy program. To date, the annual fundraiser has raised about nearly $150,000 for music therapy. It’s a community effort that involves Nazareth’s athletes, music therapy students, and others like Wilson who have a personal connection to the NICU.
The annual event also involves faculty and staff. Becky Fahy, a psychology professor at Nazareth, helps organize the event. Her now 16-year-old daughter was a Golisano NICU baby.
“Being involved is a way for my family and me to give back and support Golisano and this great program,” says Fahy, noting that her husband, Mike, a former Nazareth staff member who now works at the University of Rochester, and their daughter help out, too. “The hospital has been important to our family for a long time, and we love getting others involved in supporting it.”
She adds, “The impact of having our students get so involved is exponential. They get to see the difference they can have through service and our collective efforts also benefit the music therapy program.”
Morgan Kowalski also knows the difference music therapy can make. Her son, Tommy, was born at 25 weeks, weighing just 1lb, 11oz. He graduated from the NICU after 115 days on October 3, 2018. Kowalski met with Kong weekly once her son reached 32 weeks gestation, and their time with her quickly became the highlight of their time in the hospital.
“During our first session with Elaine, I cried,” Kowalski says. “Here I was, holding my baby like a normal mom, while this woman with the voice of a Disney princess guided me through massage and song. It was such a beautiful moment that I couldn’t hold back my tears of joy, and I am choked up as I think of it now.” Watch this video to learn more.
Support music therapy at Golisano Children’s Hospital through our crowdfunding campaign—every dollar goes toward instrument purchases, equipment upgrades, program development and expansion, and more. Your generous support for music therapy aligns with the University’s yearlong Together for Rochester campaign, too, which is designed to make life better for our broad community.
Learn more about Golisano’s music therapy program here and watch this powerful video. For even more about the program and the generosity that established it, read “The Right Notes” in the 2020 Volume 1 edition of Strong Kids, page 3.
*names changed to protect privacy
—Kristine Thompson, June 2021