Early career scientists at the University of Rochester are honing their ability to communicate their research in short, compelling, and easily understood presentations that could woo a collaborator.
Or reassure a skeptical member of the public.
In recent competitions that limited speakers to three- or five-minute talks, plus a slide or two:
Ahmed Ghazi, a surgeon and assistant professor of urology, equated the number of US deaths from medical and surgical errors to “five Boeing 747s crashing every week for an entire year.” He then described how individualized, life-like 3-D models of a patient’s organs can not only be made inexpensively, but enable surgeons to practice their operations in advance, preparing ahead of time for what might go wrong.
Ian Cero, a postdoctoral fellow in psychiatry, explained the urgent need to provide suicide prevention therapies to the growing number of people “who are balancing on a knife’s edge right now,” and yet, in the vast majority of cases, “are so distressed that they do not want to be found.” His proposal: Identify suicide clusters from Twitter and other social media, then apply algorithms to insure anonymity. In essence: “Saving lives without ever even knowing who we’re saving.”

Ghazi took first place in the University’s Falling Walls competition and will represent Rochester in a similar competition at the international conference in Berlin next month. Cero won the Steadman Family Postdoctoral Award in Interdisciplinary Research during Meliora Weekend—just as Jillian Ramos, a PhD student in biology, won first place in the University’s Three-Minute Thesis contest last spring for her presentation: “Modify or Die: When Protein Translation Goes Awry.”
All of these competitions are relatively new. They reflect the growing importance for researchers to be able to communicate with:
- Researchers in other fields. “When an engineer can talk in a language that a biologist, a humanist, and a psychologist can understand, it helps forge cross-disciplinary connections,” says Melissa Sturge-Apple, dean of graduate studies for Arts, Sciences & Engineering, whose office hosts the Steadman competition. “We can begin to see how the research in one corner of academia may inform that in another corner. It’s synergistic. This is how new discoveries are made and new scientific pursuits are born.”
- Members of the public who want to understand the research their tax dollars help fund. “Today, especially in America, there are a lot of people who are skeptical of scientific research. . . At the end of the day, our research is going to matter to them, and they need to understand that,” says Melissa Glasner, a PhD student in the cell biology of disease program, who organized this year’s Three-Minute Dissertation competition.
Cero, who has participated in multiple competitions and won at least one other, sees another advantage. “A lot of the work we do is complicated and really difficult. You’re in the nitty-gritty, you’re working through the numbers, you’re checking every statistical assumption, and it’s easy to lose sight of the big picture,” he says. “If you have to distill the work that you’re doing in five minutes and a static slide, I think it helps you think more clearly about your own work.”
Or, as Ghazi puts it: “If I can communicate the problem that I’m trying to fix in just a few minutes, that is really going to let me focus not only on the problem at hand but about where I need to go next.”
A professional development opportunity
The Steadman competition is now in its third year. Just since last year, there has been a “big improvement” in the overall quality of the presentations, says Sturge-Apple.
“I think it has to do with getting the information out about the award to our fellows and generating excitement about it,” she says. “Also, I think they are seeing this as a professional development opportunity.” The competitors were given an opportunity to work with an expert in communications and public speaking. “I thought every one of the talks this year reflected that.”
So much so that the Steadman contest judges gave two awards for second place, and there was a two-way tie for the people’s choice award. Similarly, judges at the Falling Walls competition also gave two awards for second place.
Cero, who was on debate teams in high school and college, has this advice for other researchers who want to hone their communications skills, and perhaps enter a competition themselves:
“Find a quick anecdote that summarizes the idea. The audience has to digest a lot really quickly, and that’s hard to do, even if they’re working to pay attention. In the first two or three minutes, follow some kind of emotional theme that will allow listeners to fill in the blanks as you keep talking. That tends to help a lot.”
This was Ghazi’s first such competition. He will compete against 99 other researchers and entrepreneurs from around the world at the annual Berlin conference, which commemorates the fall of the Berlin Wall. The competition highlights ideas about how to “break down walls” to overcome key challenges confronting science and society.
“You’ll see a hundred people come up with a hundred different ideas, and they all put them across in three minutes. So, it’s a beautiful snapshot of what’s going on around the world,” says Provost Rob Clark, the University’s senior vice president for research who has often attended the conference and won approval for the qualifying contest here. “For us, it’s a great opportunity to share the ideas that are underway here in Rochester.”
“It’s exciting,” Ghazi says, “but I definitely have to ramp up my game if I’m going to compete against the world in Berlin. It adds another level of anxiety, but also another level of excitement.”
Saving the lives of those who don’t want to be found —Ian Cero
Why do people die by suicide?
What made her kill herself — if you’re wondering about someone specific. Why did he take his life? And was there something that the hospital could have done on the day that he or she died?
These are questions that keep people up at night. And these are the questions that suicide researchers devote their lives to.
But unfortunately, from a prevention perspective, they are the wrong questions. Answers to why people die by suicide won’t bring our loved ones back to us, and they don’t tell us how to intervene with the people who are balancing on a knife’s edge right now.
In the United States, the suicide rate has been steadily climbing for the last 50 years. It’s now the 10th leading cause of death overall and the second leading cause of death among people under 25 — now more than doubling the number of homicides that we see every single year.
But despite the fact that the rate has been climbing, we’ve learned a lot in the last 50 years about how to help the people who come into our clinics. We now have evidence-based psychotherapies that can significantly reduce the rate of death by suicide among the people who receive them. And we even have mobile apps that have been shown to significantly reduce the rate of suicide attempts in multiple randomized control trials among their users.
Without being too cute about it, there’s an app for that. But who should we deliver those apps to?
Unfortunately, our work has been with people in clinics. And 81 percent of the people who die by suicide aren’t seen by a mental health professional within a month of their death. That means that even if our treatments were perfect, we would still lose four out of every five people we intend to save,
How to get existing life-saving treatments to the four out of every five people who are so distressed that they do not want to be found, that’s the right question.
I first became concerned about suicide and suicide research when I as working on my PhD in clinical psychology at Auburn University. I had the sense that the last 50 years of slow progress was going to continue unless we developed interdisciplinary alternatives.
There needed to be a way to mix in mathematical rigor into psychological insights.
So, alongside my PhD, I pursued a masters’ degree in statistics. I decided to do interdisciplinary research as an interdisciplinary researcher.
Over the course of that time I recognized that suicides often seem to cluster–whether it’s a spike in the rate of suicides that happen after a celebrity dies, or a large number of students who die in the same high school, all seemingly at the same time. Most of the existing research focuses on why those things happen, and what it is that we can do to prevent them. But, unfortunately, we still haven’t come up with any answers.
I decided to take a different approach. Instead of asking why those clusters happen, we should focus on harnessing them and seeing if we can make them useful for prevention.
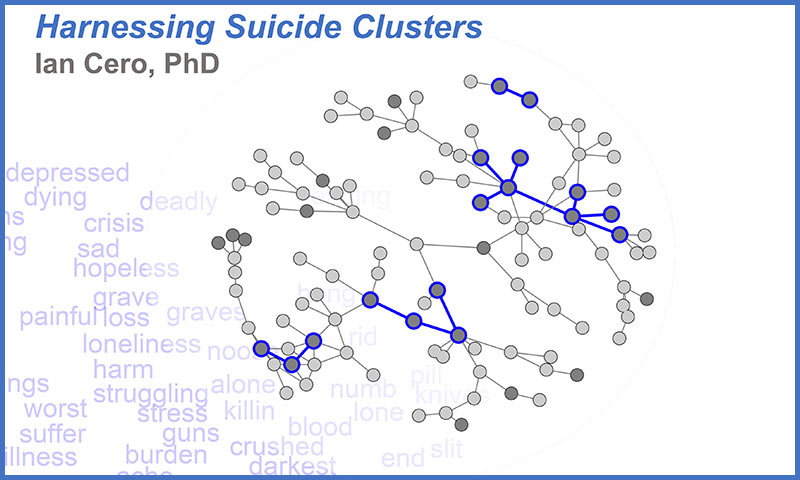
To get at that, I asked native English speakers to rate the 10,000 most common words in native English. These are words that you see behind you – depressed, dying, crisis, sad, and hopeless – for their relatedness to suicide. After we had those words stored, I programmed a $20 credit-card sized microcomputer called a Raspberry Pi to collect a one percent random sample of all the real time activity on Twitter for a two-month period. This resulted in a data set that had about 65 million posts constructed by 17 million unique users.
Each user was then flagged according to how many of these suicide-related words they had used over the course of that period. And users were regarded as linked in the network if they had reciprocally interacted with each other at least once over the course of the study period.
What you see behind you is a random subset of that 17 million user network that we were able to construct. Lightly colored nodes are people who never talked about suicide at all. Darker shaded nodes are people who talked about suicide at least once. Moreover, the dark nodes that know at least one other person who talked about suicide are circled and connected in blue.
What you are looking at here are suicide clusters rendered visible to the naked eye.
But just being able to identify these clusters isn’t enough. Could we in some way use them for prevention?
Most of the time when we perform screening to see who is at risk out there in the environment, we either screen randomly with as many resources as we can get, or we wait for people to come to us. Networks of this kind and the structures that you see in front of you, suggest that an alternative might be better.
Snowball screening – go out in the world until you find someone who is at risk. Once you find that person, screen all of their friends. Among those people who are at risk, screen their friends. And so on.
My subsequent simulations show that if we take this approach, we could more than double the number of at risk people we can find with exactly the same number of resources.
That’s a significant improvement for suicide prevention but it’s not enough on its own. If we want to be able to deliver life-saving treatments to people who don’t want to be found, we need to be able to insure their anonymity.
Which is why the next steps in my project will include using block chain technology — the same algorithms that run bitcoin — to be able to deliver these treatments to people anonymously, saving lives without ever even knowing who we’re saving.
Thank you.
Breaking the wall of surgical errors
—Ahmed Ghazi

Hello. My name is Ahmed Ghazi. I’m a surgeon by training and a student at the Warner School of Education. Today I am breaking the wall of surgical errors.
Over the past decade, the quality and safety of health care in the United States has been a point of major public concern and also a focus of significant research
Surgical and medical errors are the third leading cause of death in the United States, and multiple articles have brought this to the attention of the public. But nothing was more eye opening than an article that equated the number of deaths from medical and surgical errors to five Boeing 747s crashing every week for an entire year.
So, it’s obvious we have a problem, and for that we need a solution.
And a better way to look at the solution is to look back at another high-stakes industry that has made safer outcomes.
We all remember the Hudson Miracle, when Captain Sully (Sullenberger) was able to ditch a plane in the Hudson. He had never done this before, but he saved the lives of 191 passengers. But he was only able to do this because he practiced this over and over and over again in a very realistic environment. Unlike machines, our bodies are very different. So, if we want to create the same perfection of practice, we have to find not only a realistic but a specific customized platform for each of our patients.
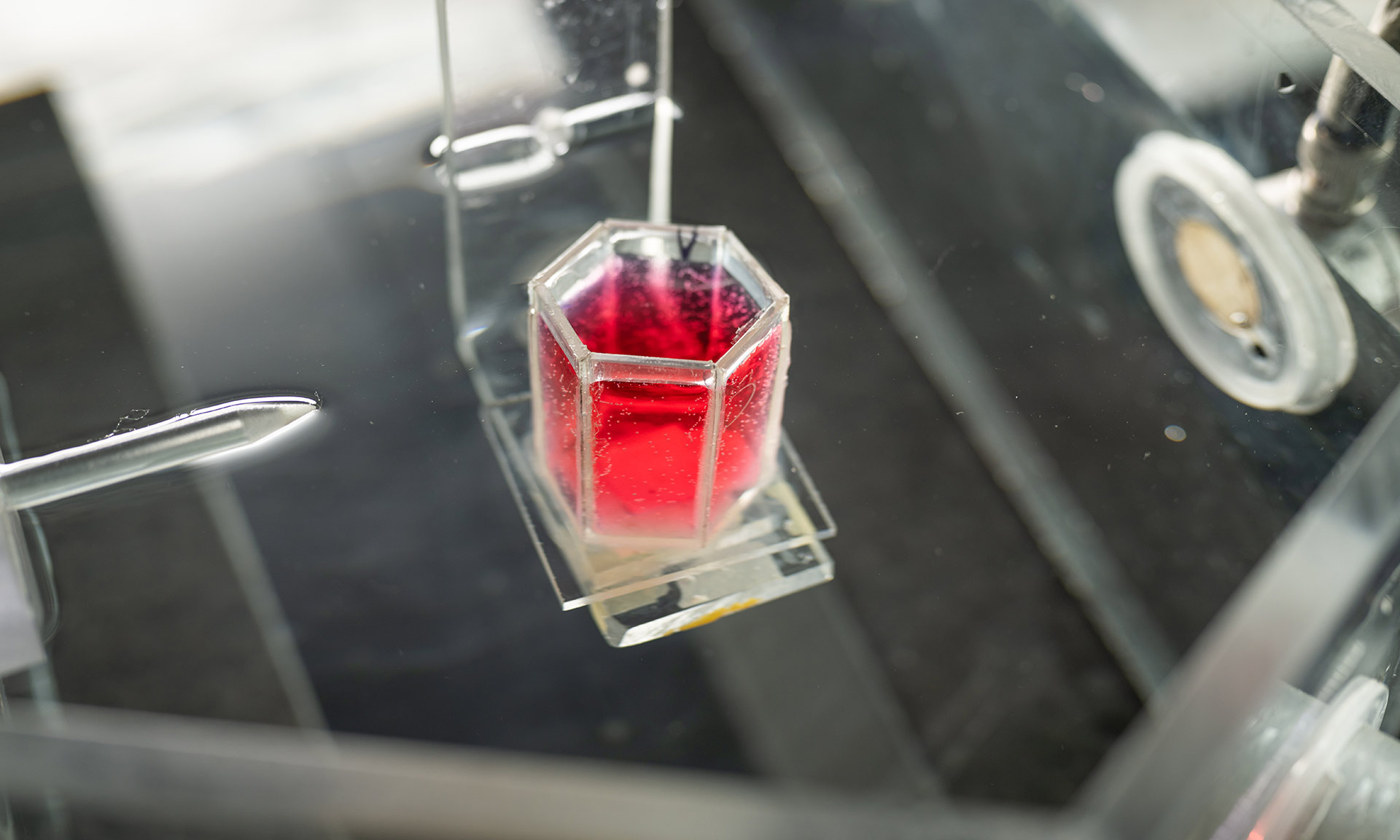
We’ve been working on this for about three years now– and yes, it does involve 3-D printing. The process starts with a patient’s image, like this one with a tumor in their kidney. Then, using a segmentation software we are able to convert that into a three-dimensional CAD, which can then send a signal over to the 3-D printer. But if I were to directly 3-D print this, it would result in a very hard plastic model—which is only a visual tool that a surgeon cannot practice on.
So, we started to print molds, which, after injecting with a hydrogel specifically formulated to replicate human properties, allowed us to create a patient-specific, realistic model.
We put that in a body cast, with all the other surrounding models that we need to do the surgery, and take it down to an operating room where a surgeon can then practice their patient’s procedure, over and over and over again, until they perfect it. The best part of this practice is that surgeons can look at the model after the fact and figure out what went right, but more importantly what went wrong – something that we would only realize as surgeons after the fact.
We’ve done this in limited number of patients and found a tremendous improvement in outcomes. The kicker here is that this is very cheap, the overhead cost is $5,000, and each model costs less than $50.
This has a huge impact not only in healthcare safety but training our future surgeons. Thank you.