Do you know a teenager who is moody or agitated, acting recklessly, sleeping too little or too much, or talking about feeling trapped? Has your child, student, or friend started to give away treasured belongings, is withdrawing, or just really behaving out of character? If so, you may want to ask outright about suicidal thoughts. Now is the time to act, say the experts.
Suicide rates have been rising in nearly every US state—and the rise is most stark among teenagers and adolescents.
In 2016, nearly 45,000 Americans age 10 or older died by suicide, according to the Centers for Disease Control and Prevention. While the rise affects every age group under 75, the strongest increase lies in the rate for girls between the ages of 10 and 14.
Researchers and clinicians have been working hand in hand to try to stem the tide of teen suicide, among them experts at the University of Rochester and the Medical Center.
“It does feel like we have our fingers on the pulse of a crisis,” says Kathleen Baynes, an assistant professor of psychiatry and a psychiatrist at UR Medicine Mental Health & Wellness. Baynes notes that her department is experiencing not only a greater volume of cases, but more complex ones as well. “We’re seeing more comorbid psychiatric issues—someone experiencing depression and another issue, like an eating disorder or substance use, someone who’s in a crisis around bullying, or loss of a family contact, a death in the family, bereavement, and on top of that, struggling with social anxiety.”
According to Michael Scharf, chief of the Division of Child and Adolescent Psychiatry at the University of Rochester Medical Center, and director of psychiatry graduate medical education, between 2015 and 2018, the hospital’s psychiatric emergency department experienced an almost 50 percent increase of children and adolescents seeking help. In the last two months, UR’s Pediatric Behavioral Health and Wellness outpatient services have received about 100 calls a week from people seeking mental health care.
Rochester follows a disturbing nationwide trend.
Research has shown that suicidal thoughts and behaviors increase dramatically during the transition to adolescence. While about 17 percent of US high school students say they have thought of suicide, more than 13 percent said they actually made a suicide plan, and 7.4 percent attempted suicide in the past year, according to the most recent CDC data.
A plethora of factors are driving this increase in teen suicide rates, including biological, psychological, and social changes that are all part of adolescence, says Cassie Glenn, an assistant professor of psychology and psychiatry, who is also a faculty member in the Center for the Study and Prevention of Suicide at the University of Rochester Medical Center.
“It is not just a phenomenon that’s observed in the US,” Glenn says. “Cross-national research from the World Health Organization shows that suicidal thoughts and behaviors are relatively rare during childhood, but increase dramatically during the transition to adolescence.”
Suicide Crisis Resources
If you or someone you know is thinking about suicide or is experiencing emotional distress, contact the Suicide Prevention Lifeline by calling 1-800-273-TALK (8255), seek help from medical or mental health professionals, or go to the nearest emergency room.
If someone shows the warning signs of suicide, do not leave the person alone. Remove any firearms, alcohol, drugs, or sharp objects that could be used in a suicide attempt and then seek professional help.
Why the increase in the suicide rate for girls aged 10 to 14?
The researchers aren’t sure why suicide rates are rising most steeply among pre-adolescent and adolescent girls. But Scharf points to factors that are affecting not just 10- to 14-year-old girls, but also older youth, such as the dramatic increase in the use of cell phones and other screens.
“It’s complicated to sort out what the real mechanisms are,” admits Scharf. While the correlation between a rise in screen time and suicide is clear, questions remain. For example, does the simple act of looking at screens increase the risk of suicidal thoughts and behaviors? Or is the cause a decrease in time spent on traditional human and social interactions? Or are changed sleep patterns as a direct consequence of more screen time to blame? Of course, the screen content itself can be troublesome, notes Scharf.
“Sometimes there can quite disturbing or even horrific bullying, or acts of cruelty that happen through the internet, through social media, or even witnessing things that could be quite traumatic, such as watching the live streaming of a suicide, or a suicide attempt,” he says.
What factors may help prevent teen suicide?
Healthy relationships and feeling connected serve as protective factors against teen suicide, says Baynes, who works with children and adolescents who’ve been hospitalized for mental illness. Struggling children and teens who have been isolated by trauma or are disconnected from their families due to other conflicts are most at risk. Part of preventing teen suicide means being able to identify vulnerable kids early and to devise effective strategies to strengthen those protective factors.
What are some risks and warning signs for suicide?
Suicide and suicidal thoughts rarely happen within a vacuum, according to experts. A whole host of factors come into play, among them external stressors such as having a parent who has engaged in suicidal behavior, a family member who has died by suicide, or the genetic contribution of a parent who has a significant psychiatric illness.
Active drug use is another contributor because it affects one’s social interactions, one’s connectedness to others, while the disinhibition and impulsivity that can happen during intoxication may play a dangerous role.
“Someone who may have recurrent thoughts of despair, or hopelessness, or that life is not worth living—while they’re under the influence of a mind-altering substance they might be more likely to act impulsively on those thoughts,” explains Scharf.
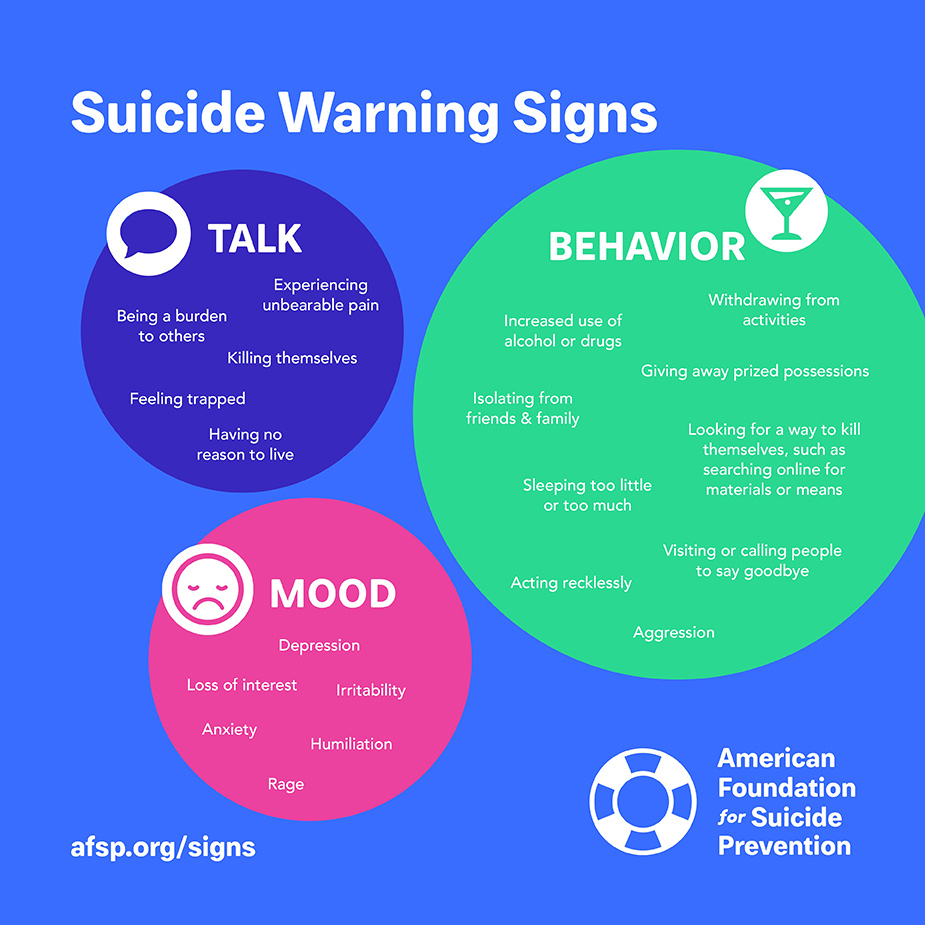
Warning signs
Experiencing unbearable pain
Being a burden to others
Killing themselves
Feeling trapped
Having no reason to live
Withdrawing from activities
Increased use of alcohol or drugs
Giving away prized possessions
Isolating from family and friends
Sleeping too little or too much
Looking for a way to kill themselves
Such as searching online for materials or means
Visiting or calling people to say goodbye
Acting recklessly
Aggression
Depression
Loss of interest
Irritability
Anxiety
Humiliation
Rage.
Warning signs that somebody might be in a suicidal crisis may look different from one person to the next, the experts caution. Look for significant changes in a person’s mood, affect, sleep patterns, and general behavior, says Glenn whose research focuses on predicting suicidal and self-injurious behaviors. Ask yourself—are you noticing significant changes such as depression, aggression, or agitation in the person?
But rather than have parents, teachers, and friends focus on a list of signs to look for, Scharf advises to look for drastic changes and to figure out why they are happening.
“I think the most important point when we’re thinking about warning signs or red flags is actually not to memorize a specific list of behaviors or statements, but instead, to really think about this person you know well, and if there’s a change, you should be curious to figure out what the change is about.”
“Ask,” echoes Baynes—and have an honest conversation. She stresses that asking about suicidal thoughts does not induce suicide.
Another common myth is that if people are talking about suicide, they’re most likely just seeking attention and not likely to act. That’s plain wrong, cautions Glenn. Talking about it, she says, is a definite red flag: “We want to know if someone is thinking about a specific suicide method. Are they researching suicide? Are they giving away possessions? Are they doing things that might indicate they’re actually moving down the pathway to engage in suicidal behavior?”
A good resource, the Rochester experts agree, are the assembled risk factors and warning signs by the American Foundation for Suicide Prevention, including health, environmental, and historical factors that up the risk. Here’s an overview of national and local resources, including at the University of Rochester Medical Center and Strong Memorial Hospital.
Research into predicting suicide
A growing body of research indicates that non-suicidal forms of self-injury—such as skin cutting or burning—are robust risk factors for predicting suicide attempts later on in adolescence, even more so than an adolescent’s own history of prior suicide attempts. Indirect self-injuring behaviors are also risk factors for teen suicide, says Glenn—such as substance use, disordered eating, or exercising to the degree that it’s intended to hurt oneself.
“Engaging in those kinds of behaviors over time might increase an individual’s tolerance for pain,” explains Glenn. “It might reduce their fear of death and that might be a potential mechanism that increases their likelihood of attempting suicide.”
Glenn is currently studying one of the most marked risk periods: both adolescents and adults are at the highest risk for suicide attempts, rehospitalization, and suicide death during the first three months after discharge following hospitalization for a suicide crisis. “We have a number of hypotheses about why that might be the case,” says Glenn. “Patients go from 24/7 care to going back into their environment, where there may be a whole host of triggers and less monitoring.”
Her team is zeroing in on how sleep disruptions during that particular period may increase suicide risk during the month immediately after hospitalization.
How do you treat youth in a suicide crisis?
Rapport-building is key to combatting teen suicide, in part because having a close and connected relationship with an adolescent helps the clinical staff figure out what’s going on internally. “Having that rapport allows us to be very thorough in terms of thinking diagnostically about who this kid is, what their symptoms are, and guiding our treatment from that point forward for a targeted therapeutic response,” says Scharf. The medical team will consider biologic illness, social factors, and educational struggles, in trying to understand what is driving the crisis.
At the same time, immediate safety needs to be addressed. In the short term, that might mean hospitalization, but with often overwhelming numbers of youngsters presenting at emergency departments, the majority of teenagers evaluated do not get admitted to the hospital. Instead, they and a trusted adult are sent home with safety plans.
That means parents may need to look at things in the home that could be easily accessed and prove fatal. “Firearms, for example, that are unsecured, or only partially, or inadequately secured, would be the most common, significant thing people should think of as potential lethal means,” says Scharf.
A good safety plan is organized around keeping someone safe in the moment, while the medical team simultaneously tries to figure out what is driving this crisis in order to help people get through it and recover.
Scharf says he really wants to dispel the myth that once someone is suicidal, they’re always suicidal. In fact, he says, data and decades of experience have shown that most suicide crises are time-limited, and they are not due to one single event, but a combination of risks and current stressors.
“If you can help people figure out how to get through that crisis and how to organize the next steps in their life around things that are important to them and meaningful to them, they’re not always suicidal,” stresses Scharf. “Help and hope are both possible, and very real.”