Mical Raz, a University of Rochester health policy expert, physician, and historian, says implementing the most up-to-date understanding of epidemiology is key to dealing effectively with pandemics like coronavirus.
The Charles E. and Dale L. Phelps Professor in Public Policy and Health, and a board-certified internist at the University’s Strong Memorial Hospital, says the United States is “lagging miserably” behind other countries in its response to the virus, is adopting many of the wrong lessons about pandemics when it comes to travel bans, and is slow in understanding the importance of social distancing.
Which current health care policies are most effective tools to try to stem the coronavirus?
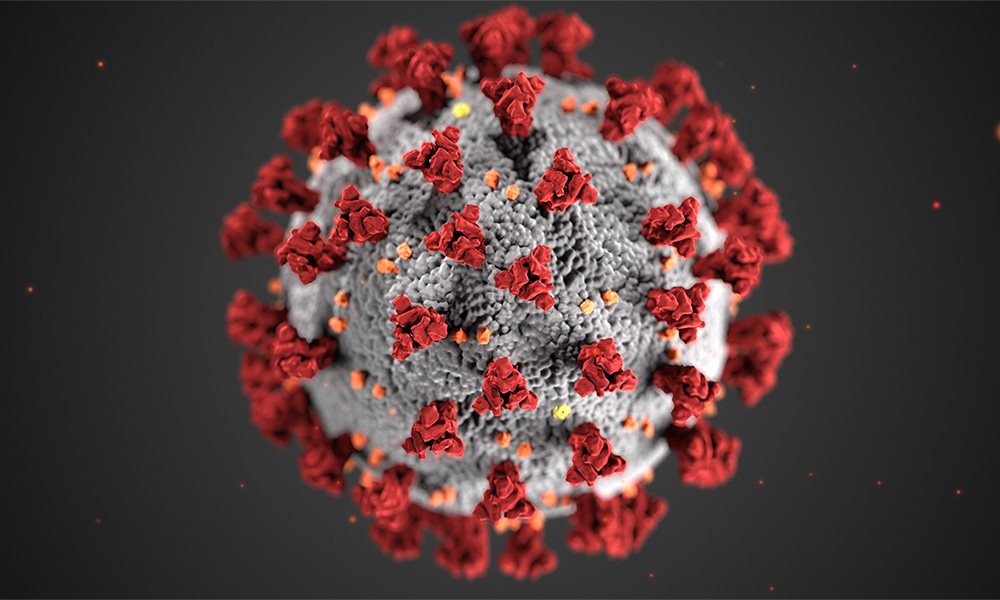
We’re in the midst of a global pandemic, and spread of the coronavirus is inevitable. The major concern is that we will see a large number of critically ill people at the same time, overwhelming our medical system response, and leading to situations akin to what Italy is currently facing—not enough ventilators to keep sick patients alive. One of the most effective steps we can take is to try and slow down the spread of the disease. People will get sick, but not all at the same time, and thus will be able to receive the care they need. Accordingly, social distancing is the policy currently in place, which holds the promise of slowing this pandemic, and hopefully curbing its spread. When people congregate in large crowded groups, the risk of infecting high numbers of people is significantly increased. Reducing social contact as much as possible will slow the spread of the disease and buy us time to both care for those in need and develop medical technologies that are needed to further deal with the pandemic.
Which health care policies historically have been most effective in dealing with past pandemics? What made little sense?
Looking at history, quarantines and plans for isolation have made sense, although, they can be seen as restrictive, coercive, and infringing on individual liberties. However, in situations of crisis and emergency, it is necessary to give up measures of our personal liberty to ensure our own well-being and that of our communities.
Politicians who have refused to act on this have unnecessarily endangered their constituents and communities. When Philadelphia leaders insisted on going forward with a large parade in 1918, they wreaked havoc and death upon their community, unleashing influenza throughout the city. Within 72 hours, all 31 hospitals in the city were full. Within six weeks, over 12,000 were dead. A few days after the parade, the city council decided to close schools, churches, and other sites of congregation. That was already too late. We should be canceling before the outbreak; canceling after is too late.
Why does comparing COVID-19 to the flu epidemic of 1918 make sense (what did we learn from it)—or make no sense (what’s different today?)
COVID-19, similar to other global pandemics, is rapidly spreading, causing high numbers of deaths, and we seem to be only at the beginning of the crisis. It is valuable to learn from comparisons to other pandemics, including the 1918 influenza epidemic, as well as the 2009 H1N1 crisis. While we have many new and advanced measures that we did not have a century ago, we currently have neither a cure nor a vaccine for the coronavirus and people are dying.
Medical technologies are fabulous, but our public health interventions have the potential for saving the most lives through prevention. Our medical technologies will likely always lag as we face new pandemics; we need to have a robust public health response and have a strong government support for evidence-based public health interventions.
What do you recommend we should all do now—individually, as an institution, in our local communities, nationally?
We need to shut down as much social interaction as we reasonably can. On Wednesday, the University of Rochester told students not to return to campus from spring break and to continue all learning remotely. That is an excellent decision, based on sound health policy. We should all be trying to contribute to slowing the spread of coronavirus by limiting social interaction, avoiding travel, reducing our exposure. Of course, washing hands is vital, and trying to maintain good hygiene—don’t touch your face, sneeze and cough into your elbows.
You have argued for the need for paid sick leave. How does that intersect with combating a pandemic?
No one should come sick to work. In order to enable that, we need paid sick leave. In general, this is good health policy. We know from multiple studies, as well as common sense, that employees without paid sick days are more likely to work sick than those who do have sick days. Sophisticated studies have shown that population spread of contagious diseases like influenza decrease when employees have access to paid sick leave.
A quarantine of 14 days, as is being recommended for coronavirus, has an enormous economic impact on workers as well as workplaces. However, in the long run, this is a good investment—and the ethical thing to do. We should encourage all sick individuals and all healthy individuals who were in touch with a known COVID-19 patient, or have other risky exposures, to self-quarantine. A number of outbreaks of COVID-19, unfortunately, have been tied to people willfully choosing to ignore these recommendations and attending social gatherings. This is compounded when the White House and some federal agencies downplay the severity of the illness and its impact on our communities. It’s time to take this as seriously as possible.
President Trump announced on Wednesday that the United States would restrict most Europeans outside of Britain from traveling to the United States for 30 days in an effort to slow the spread of coronavirus. Meanwhile, the State Department advised Americans to reconsider all international travel. Do these steps make sense?
Unfortunately the political response we received was not based on any public health evidence and does not reflect the recommendations of public health associations. People should stop unnecessary travel. That recommendation has been out there for a while. Recently the White House overruled a recommendation asking people over 65 to avoid flying at all. However, restricting flights from certain regions, but only for people from certain nationalities, makes absolutely no sense. So after President Trump’s speech on Wednesday evening three major clarifications came out—one of which is that the ban is not absolute but only affects non-nationals, so American citizens will be able to return from Europe. Of course, excluding the UK from the ban, which has a higher number of cases than some other European countries makes absolutely no sense and doesn’t address the question of people who will now fly through the UK to the US.
There are clear public health recommendations about what works and what does not. Once coronavirus is already in our community there’s no sense trying to ban people from outside our community. We should now be focusing on mitigating the effects of the virus as it travels through our communities. And there are a few evidenced-based ways to address this. Some say the White House directives are better than nothing. But doing something that is not evidence-based and does not have the potential to be useful is not better than nothing because it takes the place of doing something useful.
What ought to happen right now to slow the spread of coronavirus?
First, we need to expand our capabilities for testing. We are not testing enough. We are lagging miserably behind other countries. We cannot test everybody who needs to be tested. The initial CDC requirements in order to qualify for testing missed multiple people who later proved to be positive. We need to be able to test quickly and act on the results.
The other thing we need to do is social distancing on a scale we’re not used to in order to manage the spread. There are other things we need—doctors need enough protective equipment, and people need paid sick leave.
How does it feel right now to be a hospital physician in the trenches—so to speak?
We are well prepared and are working with the best-available evidence. We’re taking everything very seriously and we have excellent professionals who are planning for all eventualities. But we are working with the resources we have: each hospital has only a certain number of ICU beds, a certain amount of vital equipment. No hospital is equipped for a pandemic—for a massive need of expansion of treatment of critically-ill patients. And as physicians we should consider a scenario in which we may be overwhelmed by patients.
Personally, what keeps you up at night?
This is a very concerning time and we need to come to terms with the fact that our lives are going to change in ways that we cannot even anticipate. We cannot continue with our lives as has been. So, yes, I, too, lie in bed—wondering if my kids should go to their swim lesson. Right now the answer is “yes”—because there are no cases of transmission through chlorinated pool water, which might kill coronavirus. Should they go to the birthday party the next day? Probably not. I’m losing sleep over all these small decisions at each juncture, trying to make the right decisions for my family and for our communities.