The inexpensive, portable photonic chip device could help safeguard against future pandemics and detect viruses and infections in underserved populations.
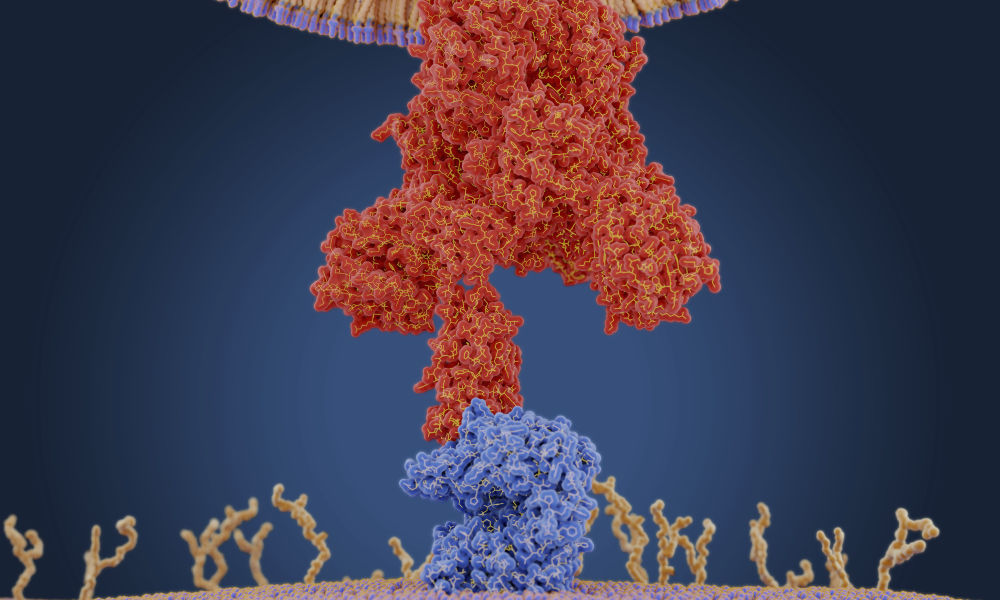
A consortium of nine industry, government, and academic partners, led by the University of Rochester, will develop the first integrated photonic sensors capable of detecting not only COVID-19 and its variants, but also other emerging viruses. The technology could even predict the severity of these and other infections.
“In two years, we want to have an advanced prototype that is ready for a company to fully commercialize,” says project director Benjamin Miller, a Dean’s Professor of Dermatology at Rochester with joint appointments in biomedical engineering, biochemistry and biophysics, optics, and materials science. “We want to have all the data ready to go so a company can pick this up and run with it.”
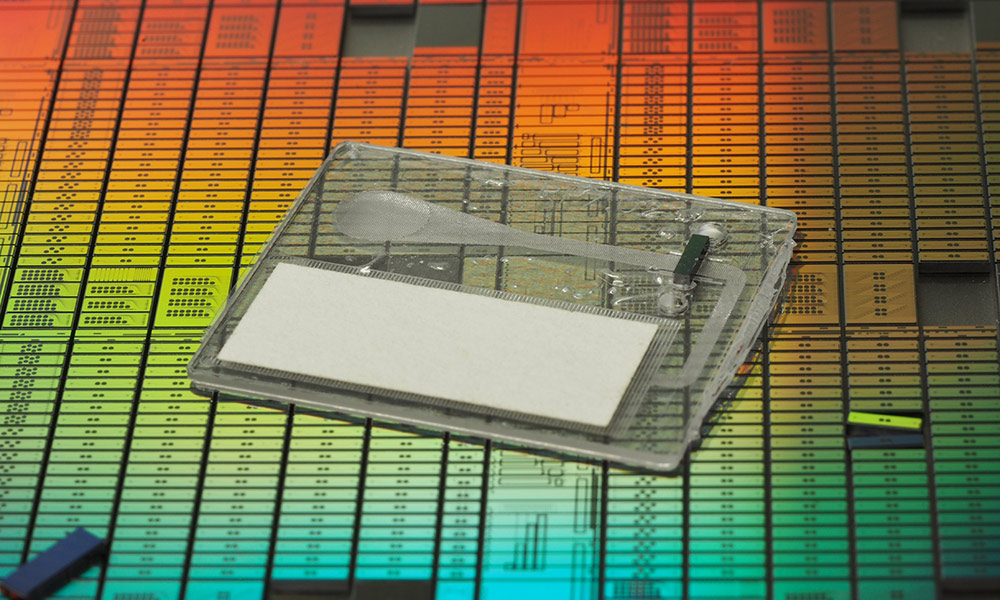
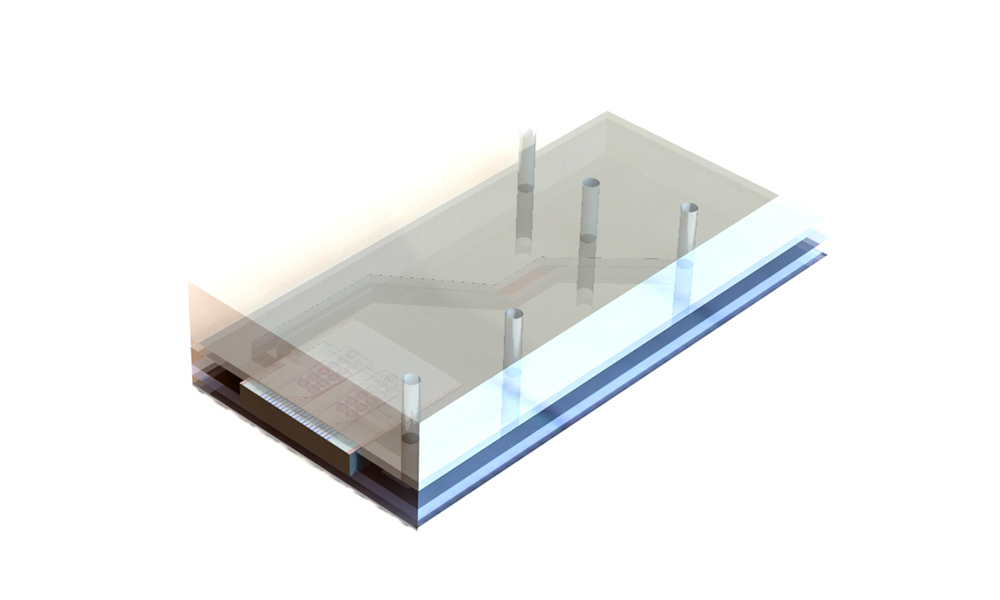
A drop of blood, serum, or saliva will be collected on an inexpensive, disposable integrated photonic chip that can then be inserted into a portable reader, producing results in one minute. The system could be used in doctors’ offices and rural or inner-city clinics.
“A major goal is to make this technology in a format that can be deployed to people who might otherwise have difficulty getting medical care,” Miller says.
The $5 million project, sponsored by AIM Photonics, is one of 13 projects nationwide to share $54 million in grants from the US Department of Commerce’s National Institutes of Standards and Technology (NIST). The goal is to improve the nation’s response to the COVID-19 pandemic and guard against future pandemics. The funding is provided by the American Rescue Act.
Tapping into diagnostic and photonics expertise nationwide
Key partners in the project include Rochester Institute of Technology (RIT), SUNY-Polytechnic Institute, Ortho-Clinical Diagnostics, Infinera, Spark Photonics, the University of California at Santa Barbara, the Naval Research Laboratory, and AIM Photonics. Syntec Optics is also participating as a subcontractor.
The partners provide a broad range of expertise in developing the tests to detect antibodies and infections, as well as in designing, fabricating, testing, and packaging integrated photonic devices.
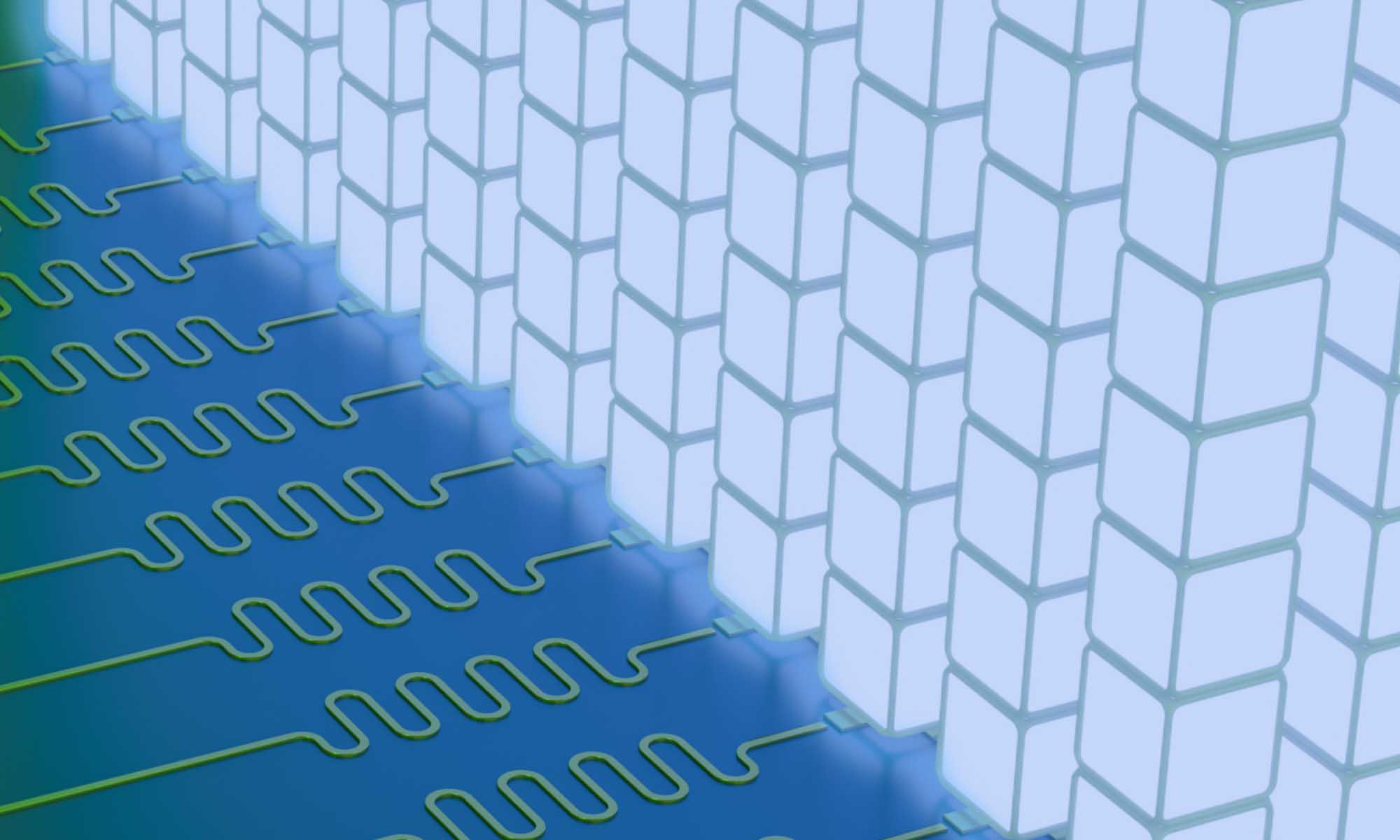
For example, the lab of Stefan Preble, professor of electrical and microelectronic engineering at RIT, will oversee the design of a laser and detector that can fit on a small photonic chip inside the reader, Miller says. This is critical to having a portable device. “It’s going to be a really exciting aspect of this project,” Miller says.
The project builds off a previous $1.7 million US Air Force–sponsored grant that Miller led involving many of the same partners. That project focused primarily on developing sensors for large analyzers in hospitals and other clinical settings.
Although that project was completed, the NIST grant will allow Miller not only to expand the team but also to take the project in a new direction.
The support from NIST for this kind of integrated photonic chip is critical, according to Miller. “First, we are at a prototype stage, in a market area for integrated photonic biosensors that is very early-stage in its development, which might make it risky for private investors,” he says. “Moreover, the diverse and nationally distributed team we have assembled is challenging to support via a traditional private-sector mechanism. This effort also allows us to focus on addressing health needs in resource-limited and underserved environments, an important societal goal.”
Support for pandemic-fighting photonic chip
Miller also thanked US senators Charles Schumer and Kirsten Gillibrand and Congressman Joe Morelle for their “incredible support.”
“This funding furthers our efforts to develop the first disposable integrated photonic sensors capable of detecting not only COVID-19 and its variants, but other emerging viruses. Doing so without federal support would have been challenging and furthers the goal of creating a quick, affordable diagnostic tool that is easily accessible to aid in the nation’s fight against the current pandemic and future ones.”
Schumer says, “As lead negotiator of the American Rescue Plan, I’m proud that funding I helped secure will be used by the University of Rochester for cutting-edge, potentially lifesaving new technology. University of Rochester’s research will not only help us continue to attack the Covid pandemic head-on, but it will also boost jobs and better prepare us for emerging viruses moving forward. I’m delighted that these efforts will take place in Rochester and across New York State, and I look forward to seeing the nationwide impacts University of Rochester’s work will have on our communities.”
“The University of Rochester has long been a leader in world-class research, and I’m thrilled they have received this significant award that underscores their important work,” says Morelle. “Not only is their work critical to strengthening our economy, it is helping our local efforts to fight this pandemic and revitalize our communities. I’m proud to have secured funding for this grant through the American Rescue Plan and I look forward to our continued work together to strengthen our manufacturing economy.”
Read more
‘Organ on a chip’ is the wave of the future
Rochester researchers are building technology to predict the course of tendon injuries—a form of personalized medicine that will lead to more effective treatments.
 Study finds evidence of COVID-19 antibodies in breast milk of vaccinated mothers
Study finds evidence of COVID-19 antibodies in breast milk of vaccinated mothers
Medical Center researchers have found that mothers with both disease-acquired and mRNA vaccination-acquired immunity to COVID-19 produced breast milk with active SARS-CoV-2 antibodies.
 COVID-19: What’s RNA got to do with it?
COVID-19: What’s RNA got to do with it?
Rochester research into RNA structure and function provides key information for developing coronavirus treatments.