A person who has a stroke that causes vision loss is often told there is nothing they can do to improve or regain the vision they have lost.
But research from the University of Rochester, published in the journal Brain, may offer hope to stroke patients in regaining vision.
The Rochester team found that survivors of occipital strokes—strokes that occur in the occipital lobe of the brain and affect the ability to see—may retain some visual capabilities immediately after the stroke, but these abilities diminish and eventually disappear permanently after approximately six months. By capitalizing on this initial preserved vision, early vision training interventions can help stroke patients recover more of their vision loss than if training is administered after six months.
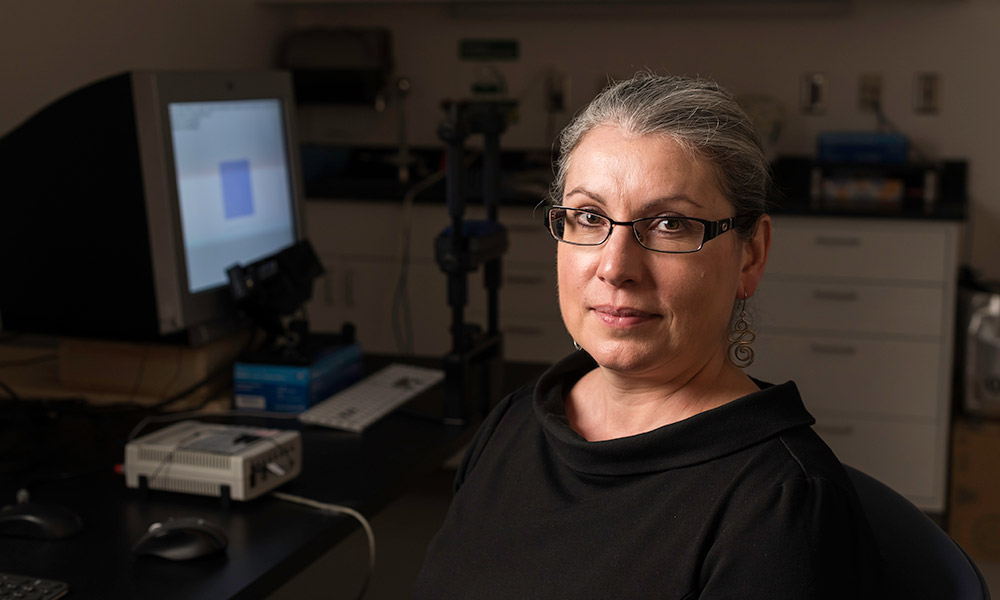
“One of our key findings, which has never been reported before, is that an occipital stroke that damages the visual cortex causes gradual degeneration of visual structures all the way back to the eyes,” says Krystel Huxlin, the James V. Aquavella, MD Professor in Ophthalmology at the University of Rochester’s Flaum Eye Institute.
The Rochester research team—including Elizabeth Saionz, a PhD candidate in Huxlin’s lab and the first author of the paper; Duje Tadin, professor and chair of the Department of Brain and Cognitive Sciences; and Michael Melnick, a postdoctoral associate in Tadin and Huxlin’s labs—also discovered that early intervention in the form of visual training appears to stop the gradual loss of visual processing that stroke victims may experience.
Vision stroke rehabilitation remains a developing field, and previous studies and trials of experimental therapies have focused on patients with chronic vision loss—that is, patients who are more than six months post-stroke.
“Right now, the ‘standard of care’ for vision stroke patients is that they don’t receive any targeted therapy to restore vision,” Saionz says. “They might be offered therapy to help maximize use of their remaining vision or learn how to navigate the world with their new limited vision, but there are no treatments offered that can give them back any of the vision that they lost.”
The new study compared chronic patients—those who were more than six-months post-stroke—with early subacute patients, who started training within the first three months after their stroke.
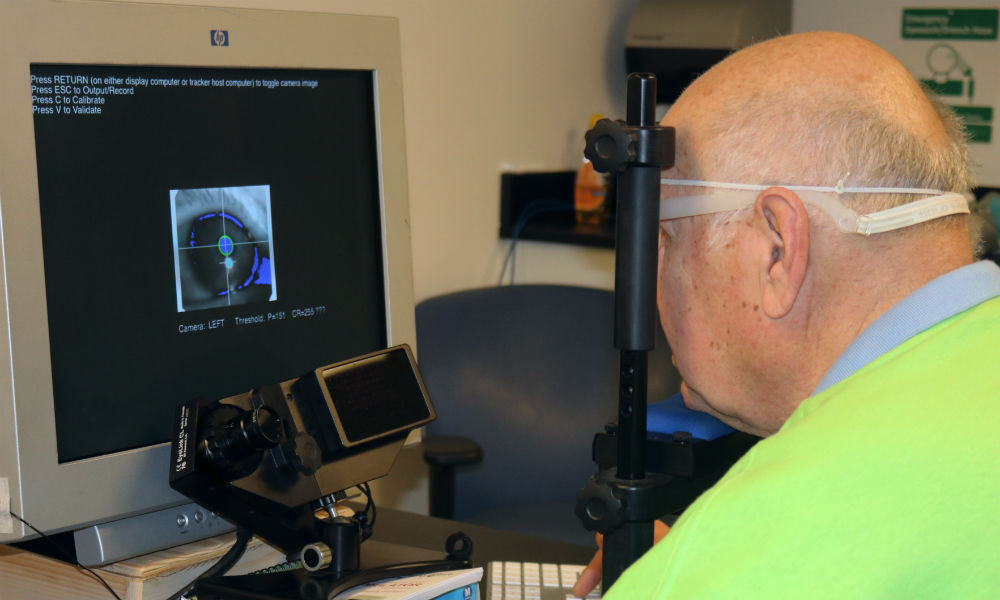
The researchers trained both groups of stroke patients using a computer-based device Huxlin developed. The training is a form of physical therapy for the visual system and involves a set of exercises that stimulates undamaged portions of the visual cortical system to use visual information. With repeated stimulation, these undamaged parts of the brain can learn to more effectively process visual information that is not filtered by the damaged primary visual cortex, partially restoring conscious visual sensations.
The researchers discovered that the subacute patients who underwent such vision training recovered global motion discrimination—the ability to determine the direction of motion in a noisy environment—as well as luminance detection—the ability to detect a spot of light—faster and much more efficiently than the chronic patients.
Overall, the group’s findings suggest that individuals may maintain visual abilities early after a stroke, indicating they have preserved some sensory information processing that may temporarily circumvent the permanently damaged regions of the brain. Early visual training may therefore be critical both to prevent vision from degrading and to enhance restoration of any preserved perceptual abilities.
“For the first time, we can now conclusively say that just as for sensorimotor stroke, ‘time is vision’ after an occipital stroke,” Huxlin says.
The study was funded by the National Institutes of Health, including NIH’s National Eye Institute, National Center for Advancing Translational Sciences, and National Institute of General Medical Sciences, as well as the Research to Prevent Blindness Foundation.
Editor’s note: As of 2024, the therapy discussed below remains experimental and is available only as part of a clinical trial. You can register via ClinicalTrials.gov or email christine_callan@urmc.rochester.edu to find out more about ongoing or upcoming trials.