Rochester researchers are developing multimodal, non-invasive ways to study the brain’s physiology and reduce neurological issues associated with the therapy.
Extracorporeal membrane oxygenation (ECMO) can be a life-saving therapy for patients with acute heart or lung failure. During ECMO therapy, a patient’s blood flows out of their veins through tubes and into a machine that does both the actions of the heart and lungs. The oxygenated blood is then returned to the body allowing the heart and lungs to rest.
While ECMO can stabilize a critically ill patient in an intensive care unit, the procedure carries significant risks, including brain injury. Often these patients are comatose, and current neuromonitoring techniques are too risky and invasive to perform routinely. Now, researchers at the University of Rochester are devising new non-invasive, multimodal techniques to monitor the brain’s physiology and prevent harm.
Regine Choe, an associate professor of biomedical engineering and of electrical and computer engineering, and Imad Khan, an assistant professor of neurology and neurosurgery, have linked together multiple devices to evaluate different aspects of the brain’s health. The devices monitor the cortex, the brain’s outermost layer where neurons reside, using electroencephalography (EEG) to study electrical activity and a new optical method called diffuse correlation spectroscopy (DCS), which measures brain-blood flow. They also use evoked potentials—measurements of the electrical signals produced by the nervous system in response to an external stimulus— to examine deeper structures in the brain.

“Using near-infrared light, we can non-invasively evaluate blood flow about one centimeter into the brain tissue,” says Choe. “This is done by bouncing light off the red blood cells in the brain’s capillaries.”
She adds, “The correlation between blood flow measured by DCS and neural activity measured by EEG can tell us a lot about the health of the brain. We believe evoked potentials will provide important indicators about whether a patient can potentially wake up from their coma.”
ECMO therapy—enhanced with more data
The project began in 2019 with funding from a University Research Award and the team has tested it on more than 20 patients to date. Choe and Khan recently received a National Institutes of Health grant to further refine their method. The grant will allow them to test the process on 100 comatose patients who have suffered from cardiac arrest, some of whom are receiving ECMO and others who are not.
So far, the researchers have used DCS on the front portions of the brain, which has yielded intriguing findings such as asymmetric perfusion in the brain’s hemispheres. This finding may be caused by ECMO in patients who are comatose. The researchers want to expand perfusion monitoring to the 20 locations of the brain often used for EEG monitoring, thereby providing an additional metric for brain health. They aim to create a low-cost instrument incorporating both modalities that they can prepare for clinical trials.
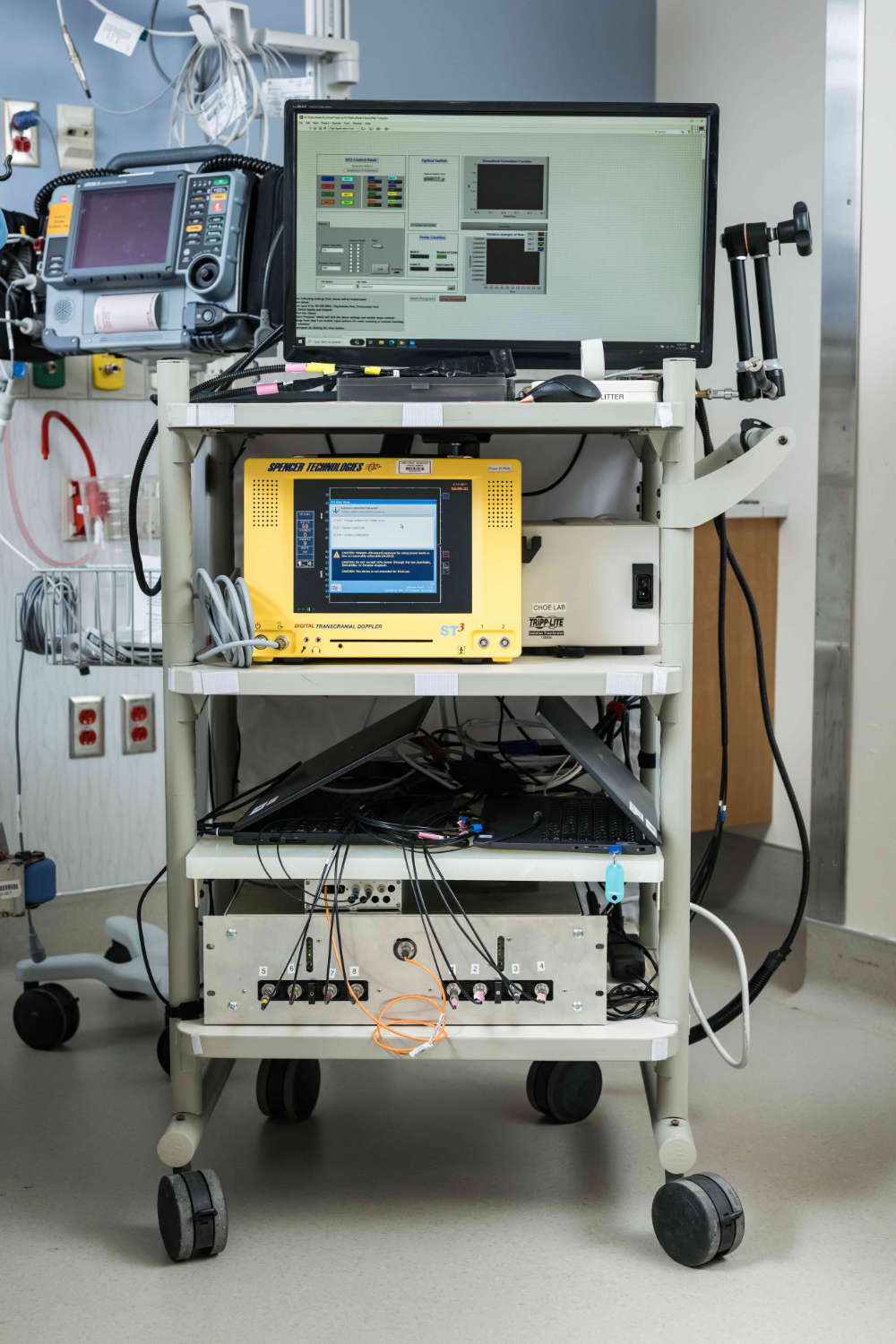
The researchers say the data they collect through their system will provide important information to help clinicians optimize ECMO therapy.
“Our brains naturally have extremely intricate ways of controlling the amount of blood flow it receives, and how much oxygen and carbon dioxide need to be in the blood,” says Khan. “With ECMO, we are bypassing all of that to put blood flow and gas exchange in the hands of a clinician. Our device will provide clinicians with more data to make informed decisions about how to regulate these factors.”
Mark Marinescu, an assistant professor of clinical medicine and a cardiac intensivist collaborating on the project, believes the technique can help provide better care to patients and their families.
“A lot of times patients will come in unconscious because they are so sick and you have to make life-changing decisions about long-term medical devices to support them,” says Marinescu. “It would be really helpful to be able to predict if they are neurologically going to do okay afterwards. That would help us counsel patients’ families regarding what we should advocate for.”